AVF thrombosis:(HD)
- timing: during or before or after ?
- possible for doing HD via that AVF?
- evaluation: thrill, bruit, doppler, and so on.
HX + P/EX = QRAAA + ASSOCIATED + OPDC + P/EX
- generally: total occlusion, acute occlusion
- if it's not totally occluded
= no urgent intervention needed(Evaluation on Monday would be good enough)
= no heparin infusion needed.
- no de-clot over the weekend per IR.
- MOSTLY => EVALUATION on MONDAY(Vascular = no urgent -> IR = Monday !, something like that....)
2018년 12월 28일 금요일
2018년 12월 27일 목요일
[CK] Higher dose ASPIRIN in CABG populations !!!? [ Q]
The researchers also found that the majority of coronary artery bypass graft (CABG) patients received low-dose aspirin, even though guidelines call for the use of high-dose aspirin in this population.
Findings from the analysis point to the need for large-scale efforts to educate clinicians and patients about the benefits of low-dose aspirin in the secondary prevention of acute coronary syndrome, the researchers noted.
"Wide variability in the proportional use of high-dose aspirin across centers suggests significant influence from local practice habits and uncertainty about appropriate aspirin dosing," Das and co-authors wrote.
https://www.medpagetoday.com/primarycare/obesity/47185
Daily Basic [CK] JVP and EKG with rhythm(닥터노)
Capillary refill: 5-7secs holding => should be returned 2 sec.
Hepatojugular Reflux (HJR)
Hepatojugular reflux is the distension of the neck veins precipitated by the maneuver of firm pressure over the liver. It is seen in tricuspid regurgitation, heart failure due to other non-valvular causes, and other conditions including constrictive pericarditis, cardia tamponade, and inferior vena cava obstruction. The HJR maneuver may be performed as follows:
- The patient is positioned supine with elevation of the head at 45 degrees.
- Look at jugular pulsations during quiet respirations (baseline JVP).
- Apply gentle pressure (30-40 mm Hg) over the right upper quadrant or middle abdomen for at least 10 seconds (some suggest to 1 minute).
- Repeat the JVP.
- An increase in JVP of >3 cm is a positive HJR test.
Note: Normal subjects will have a decrease in JVP with this maneuver since venous return to the heart will be reduced. The jugular venous pressure may transiently rise and then return to normal or decrease within 10 seconds.
Or you can also go to Evidence Base for more data.
; physical exam
JVP: 8cm = normal(3cm + 5cm)
Hepatojugular reflex = +3cm more. = >6cm = positive sign.
[ ] NEXT _ CARDIAC MURMUR !!!!!
2018년 12월 25일 화요일
[CK] [ ] Q oxyhemoglobin curve. MVO2 > 70% as our goal !(65% - 70%)
OxyHemoglobin Dissociation Curve
This curve describes the relationship between available oxygen and amount of oxygen carried by hemoglobin.
- The horizontal axis is Pa02, or the amount of oxygen available.
- The vertical axis is SaO2, or the amount of hemoglobin saturated with oxygen.
- Once the PaO2 reaches 60 mm Hg the curve is almost flat, indicating there is little change in saturation above this point.
- So, PaO2 of 60 or more is usually considered adequate.
- But, at less than 60 mm Hg the curve is very steep, and small changes in the PaO2 greatly reduce the SaO2.
- The term "affinity" is used to describe oxygen's attraction to hemoglobin binding sites.
- Affinity changes with:
- variation in pH,
- temperature,
- CO2 and,
- 2,3,-DPG
- a metabolic by-product which competes with O2 for binding sites.
- Traditionally the curve starts with:
- pH at 7.4,
- temperature at 37 Centigrade, and
- PaCO2 at 40.
- Changes from these values are called "shifts".
Click a button to shift the curve.
- Affinity changes with:
- A left shift will increase oxygen's affinity for hemoglobin.
- In a left shift condition (alkalosis, hypothermia, etc.) oxygen will have a higher affinity for hemoglobin.
- SaO2 will increase at a given PaO2, but more of it will stay on the hemoglobin and ride back through the lungs without being used. This can result in tissue hypoxia even when there is sufficient oxygen in the blood.
- A right shift decreases oxygen's affinity for hemoglobin.
- In a right shift (acidosis, fever, etc.) oxygen has a lower affinity for hemoglobin. Blood will release oxygen more readily.
- This means more O2 will be released to the cells, but it also means less oxygen will be carried from the lungs in the first place.
ARTERIAL: 90%
MIXED VENOUS: SvO2(pulmonary artery <- including coronary sinus)
> 60%(SCVo2 > 70%)

OXYGEN: ScvO2 and SvO2
Hemoglobin in arterial blood is highly saturated with oxygen (SaO2). Normal levels of SaO2 delivered to tissues are 95 - 98%.
Central venous (ScvO2) and mixed venous oxygen saturation (SvO2) are measurements of the relationship between oxygen consumption and oxygen delivery in the body. Normal values of mixed venous oxygen saturation (SvO2) are 60 - 80%. Central venous oxygen saturation (ScvO2) values represent regional venous saturations with a normal value of ~70%. ScvO2 usually measures slightly higher than SvO2 as it has not mixed with the venous blood from the coronary sinus. Although the values may differ, they trend together.
Hemoglobin in arterial blood is highly saturated with oxygen (SaO2). Normal levels of SaO2 delivered to tissues are 95 - 98%.
Central venous (ScvO2) and mixed venous oxygen saturation (SvO2) are measurements of the relationship between oxygen consumption and oxygen delivery in the body. Normal values of mixed venous oxygen saturation (SvO2) are 60 - 80%. Central venous oxygen saturation (ScvO2) values represent regional venous saturations with a normal value of ~70%. ScvO2 usually measures slightly higher than SvO2 as it has not mixed with the venous blood from the coronary sinus. Although the values may differ, they trend together.
| OXYGEN: BALANCE Oxygen balance is necessary to sustain life. SvO2 is the "watchdog" of this balance and is often called the "fifth vital sign." When monitored, it serves as an early trouble indicator and can help clinicians adjust therapies. It is also a means of interpreting other clinical variables. In a healthy individual, normal SvO2 is between 60 percent and 80 percent.
|
OXYGEN: BALANCING SUPPLY AND DEMAND <=> CARDIOGENIC SHOCK + SEPSIS !!! BOTH CAN DECREASE IT . When the oxygen supply and demand balance is threatened, the body will compensate in the following three ways: Increased cardiac output and/or heart rate:
|
GLOBAL TISSUE HYPOXIA An indicator of serious illness, global tissue hypoxia is a key development preceding multiorgan failure and death. In cases of circulatory abnormalities, an imbalance between systemic oxygen delivery and oxygen demand, results in global tissue hypoxia. |
2018년 12월 24일 월요일
[CK] Dyspnea method
fentanyl inhalation: single-dose inhalation of nebulized fentanyl citrate (250 mcg)
fentanyl neb
- 25mcg q 3hr inhalation.
Intravenous* sedative and analgesic dosing regimens for managing pain, agitation, and delirium in the intensive care unit
https://www.uptodate.com/contents/image?imageKey=PULM%2F79667&topicKey=PULM%2F2888&search=fentanyl%20inhal&rank=2~150&source=see_link
fentanyl neb
- 25mcg q 3hr inhalation.
Intravenous* sedative and analgesic dosing regimens for managing pain, agitation, and delirium in the intensive care unit
https://www.uptodate.com/contents/image?imageKey=PULM%2F79667&topicKey=PULM%2F2888&search=fentanyl%20inhal&rank=2~150&source=see_link
[CK] hematoma = 1-4weeks - resolution(any hemorrhage = 3 weeks at least)
. The swelling and pain of the hematoma will go away. This takes from 1 to 4 weeks, depending on the size of the hematoma
2018년 12월 23일 일요일
[CK] isolated conjunctival injury without trauma = easy.
Management of isolated conjunctival injuries are as follows (see 'Management' above):
•Spontaneous, nontraumatic causes of subconjunctival hemorrhage self-resolve over two to three weeks without ocular sequelae and require no treatment. In elderly patients, the clinician should perform a complete history to determine if any trauma occurred and measure the blood pressure. Coagulation studies should be performed to assess for a bleeding diathesis or overmedication in patients who are anticoagulated if subconjunctival hemorrhages are recurrent.
•Subconjunctival hemorrhage resulting from trauma (or cases when trauma cannot be ruled out in patients who are poor historians), particularly in the setting of bullous elevation of the conjunctiva, warrants ophthalmology consultation to evaluate for underlying retinal trauma and definitively rule out open globe injury.
•Patients with conjunctival abrasions are treated with antibiotic ointment (eg, erythromycin ophthalmic ointment) and for patients whose symptoms have not fully resolved within one to three days or contact wearers, referral to an ophthalmologist.
•Patients with small (<1 cm) conjunctival lacerations not associated with an open globe should receive an antibiotic ointment (eg, erythromycin ophthalmic ointment) with ophthalmologic follow up arranged for one to three days. Lacerations larger than 1 cm should be promptly referred to an ophthalmologist.
•Superficial conjunctival foreign bodies can be removed at the slit lamp with the aid of a cotton-tipped applicator after the instillation of topical anesthetic (eg, proparacaine). Alternatively, multiple or loose foreign bodies may be removed with normal saline irrigation.
[Q] CHEST TUBE CHECKLIST
? Orange - suction
? Air = leakage or air suction
? Tidling = on the pleural space
? Air = leakage or air suction
? Tidling = on the pleural space
2018년 12월 22일 토요일
[CK] Right Cardiac Cath, Pulmonary vascular resistacne( >3 WU)
The standard definition of pulmonary hypertension is defined by most experts as a mean pulmonary arterial pressure of = 25 mm Hg, with a concomitant pulmonary capillary wedge pressure of = 15 mm Hg, and pulmonary vascular resistance of > 3 Wood units. These criteria are derived from the National Institutes of Health (NIH) registry of patients with primary pulmonary hypertension, now known as idiopathic pulmonary arterial hypertension (IPAH).3
https://www.uptodate.com/contents/pulmonary-hypertension-in-patients-with-left-heart-failure?search=mixed%20pulmonary%20hypertension&source=search_result&selectedTitle=4~150&usage_type=default&display_rank=4
 \
\
LA(PCWP): 14
LV 120/14
RA: 7
RV: 25 <---6---> PA: (mean 16), 25
SVR: 800-1200
PVR: 3WU.
Transpul. gra: <6
https://www.uptodate.com/contents/pulmonary-hypertension-in-patients-with-left-heart-failure?search=mixed%20pulmonary%20hypertension&source=search_result&selectedTitle=4~150&usage_type=default&display_rank=4
 \
\LA(PCWP): 14
LV 120/14
RA: 7
RV: 25 <---6---> PA: (mean 16), 25
SVR: 800-1200
PVR: 3WU.
Transpul. gra: <6
2018년 12월 20일 목요일
[CK] CP with RECENT AMI(3yo)
Any record of AMI during this 3-year period was categorised as a recent AMI.
2018년 12월 19일 수요일
[CK] Tube feeding -gradual + Q4HR residual. (250, 500 - residual => hold or stop) . 30cc -> q6hr 30cc/hr without 400 residual to goal.
2. Assess tolerance of tube feedings.
A. Check stool amount and frequency daily.5
B. Check gastric residual every 4 hours during the first 48 hours of feeding in gastrically
fed patients.
When goal rate is attained, it is possible to reduce gastric residual monitoring to every 6-8 hours in patients who are not critically ill.
Continue to assess gastric residuals in critically ill patients every 4 hours.
High or increasing gastric residuals often are symptoms of problems that are not associated with tube feeding. Therefore, it is important to investigate other causes of high-gastric residual volumes rather than simply holding the tube feeding.
The recommendations of the American Society for Parenteral and Enteral Nutrition (A.S.P.E.N.) regarding gastric residuals are as follows:
• If the gastric residual volume (GRV) is >250 mL after a second gastric residual check, consider a promotility agent in adult patients.
• A GRV >500 mL should result in holding enteral nutrition and reassessing patient tolerance by use of an established algorithm, including physical assessment, GI assessment, evaluation of glycemic control, minimization of sedation, and consideration of promotility agent use, if not already prescribed.
cf) Note signs and symptoms that may indicate GI intolerance, including abdominal distension, vomiting, diarrhea, or constipation; assess non-tube feeding factors that may contribute to gastrointestinal symptoms in patients on tube feeding (see Potential Problems and Preventive Actions, p 14-17) before changing type, amount, or rate of feeding.
UPTODATE:
When goal rate is attained, it is possible to reduce gastric residual monitoring to every 6-8 hours in patients who are not critically ill.
Continue to assess gastric residuals in critically ill patients every 4 hours.
High or increasing gastric residuals often are symptoms of problems that are not associated with tube feeding. Therefore, it is important to investigate other causes of high-gastric residual volumes rather than simply holding the tube feeding.
The recommendations of the American Society for Parenteral and Enteral Nutrition (A.S.P.E.N.) regarding gastric residuals are as follows:
• If the gastric residual volume (GRV) is >250 mL after a second gastric residual check, consider a promotility agent in adult patients.
• A GRV >500 mL should result in holding enteral nutrition and reassessing patient tolerance by use of an established algorithm, including physical assessment, GI assessment, evaluation of glycemic control, minimization of sedation, and consideration of promotility agent use, if not already prescribed.
cf) Note signs and symptoms that may indicate GI intolerance, including abdominal distension, vomiting, diarrhea, or constipation; assess non-tube feeding factors that may contribute to gastrointestinal symptoms in patients on tube feeding (see Potential Problems and Preventive Actions, p 14-17) before changing type, amount, or rate of feeding.
UPTODATE:
Amount and rate — The daily amount of enteral nutrition is tailored to the nutritional and fluid needs of each patient. A calorie goal of 18 to 25 kcal/kg/d is a reasonable initial range to use to meet the needs of a critically ill patient of normal weight. In practice, it is generally considered acceptable that enteral feeding be initiated in critically ill patients at a rate of 10 to 30 mL/hour (for standard enteral formulations), so called "trophic" feeding, for six days and then incrementally increased to the target rate. It is our practice to initiate feeds at 25 to 30 percent of estimated goal rate.
In patients who are subjectively more critically ill, we do not attempt to increase further toward goal until the fifth to seventh day of critical illness. In less critically ill patients, advancement is made toward goal as tolerated, based on gastrointestinal symptoms and physical examination (ie, presence of abdominal distension).
We do not use gastric residuals, unless greater than 500 mL, as criteria for tolerance, and are working toward cessation of routinely checking gastric volume (see 'Monitoring' below). Provided the enteral nutrition is paused infrequently, for issues such as gastric distension, diarrhea, or vomiting, this suggested approach should result in the patient ultimately reaching a stable target rate within a reasonable period of time.
START WITH 25cc/hr -> increase 25/hr q6hr unless residual >400.
Or: low-volume enteral feeding consisted of initiating enteral feeding at approximately 10 to 30 mL per hour (approximately 30 percent of the maintenance target), continuing that rate for six days, and then advancing the infusion rate using the same protocol that was used in the full enteral feeding group. = better outcome with low rate.
(30cc -> uptitrate 30cc q 6hr for now.)
2018년 12월 6일 목요일
[CK] Diastolic failure (ASE/EACVI guideline standards.
[normal value]
E' >7(med), >10(lateral)
E/E' <14(Ave), 15(med)
TR velocity < 2.8
LAVI < 34
====================
>1 abnormal = normal
>2 abnormal = intermediate
>3 abnormal = DIASTOLIC DYSFUNCTION.
Point
1. Abnormal LV relaxation(tau = in cath, e' = tissue doppler) = 1st manifestation of diastolic dysf.
2.E/e' = specific for increased filling pressure. >15 (low e' = impaired relaxation. not eleastic. stiff= slow relax.... delayed relax...) <-> DT: faster shift; +high E = high P. and which affected by preload as well. E ~ related to stiffness(stiff = slow E, but high volume = high E) So It's reliabel
PRESSURE + RELAXATION ! => 2 can be measured with ECHOCARDIOGRAM(reliable like cardiac cath !)
========================
Grade
Normal =====> Smallest size of normal pattern = grade 3. E>A, e'>a'
Grade 1 = abnormal E<A, e'<a' => totally opposite = easy to diagnosis !!! Grade 1 완전반대. 얘만 그렇다!!!!!
Grade 2 = mixed = pseudonormalization of flow E>A, but still e'<a'
Grade 3 = normali like E>A, e'>a' but too small.
E' >7(med), >10(lateral)
E/E' <14(Ave), 15(med)
TR velocity < 2.8
LAVI < 34
====================
>1 abnormal = normal
>2 abnormal = intermediate
>3 abnormal = DIASTOLIC DYSFUNCTION.
Point
1. Abnormal LV relaxation(tau = in cath, e' = tissue doppler) = 1st manifestation of diastolic dysf.
2.E/e' = specific for increased filling pressure. >15 (low e' = impaired relaxation. not eleastic. stiff= slow relax.... delayed relax...) <-> DT: faster shift; +high E = high P. and which affected by preload as well. E ~ related to stiffness(stiff = slow E, but high volume = high E) So It's reliabel
PRESSURE + RELAXATION ! => 2 can be measured with ECHOCARDIOGRAM(reliable like cardiac cath !)
========================
Grade
Normal =====> Smallest size of normal pattern = grade 3. E>A, e'>a'
Grade 1 = abnormal E<A, e'<a' => totally opposite = easy to diagnosis !!! Grade 1 완전반대. 얘만 그렇다!!!!!
Grade 2 = mixed = pseudonormalization of flow E>A, but still e'<a'
Grade 3 = normali like E>A, e'>a' but too small.
2018년 12월 5일 수요일
[CK] VBG vs ABG(blood gas)
CORRELATION BETWEEN VBG AND ABG
pH
- Good correlation
- pooled mean difference: +0.035 pH units
pCO2
- good correlation in normocapnia
- non-correlative in severe shock
- 100% sensitive in detecting arterial hypercarbia in COPD exacerbations using cutoff of PaCO2 45 mmHg and laboratory based testing (McCanny et al, 2012), i.e. if VBG PCO2 is normal then hypercapnia ruled out (PaCO2 will be normal), though this conflicts with the meta-analysis by Byrne et al 2014 (see below)
- correlation dissociates in hypercapnia – values correlate poorly with PaCO2 >45mmHg
- Mean difference pCO2 +5.7 mmHg (wide range in 95%CIs among different studies, on the order of +/-20 mmHg)
- A more recent meta-analysis by Byrne et al, 2014 found that the 95% prediction interval of the bias for venous PCO2 was −10.7 mm Hg to +2.4 mm Hg. They note that in some cases the PvCO2 was lower than the PaCO2. The meta-analysis had considerable heterogeneity between studies which limits the reliability of its conclusions.
HCO3
- Good correlation
- Mean difference −1.41 mmol/L (−5.8 to +5.3 mmol/L 95%CI)
Lactate
- Dissociation above 2 mmol/L
- Mean difference 0.08 (-0.27 – 0.42 95%CI)
Base excess
- Good correlation
- Mean difference 0.089 mmol/L (–0.974 to +0.552 95%CI)
PO2
- PO2 values compare poorly
- arterial PO2 is typically 36.9 mm Hg greater than the venous with significant variability (95% confidence interval from 27.2 to 46.6 mm Hg) (Byrne et al, 2014)
- See also: Central venous oxygen saturation (ScvO2) monitoring, mixed venous oxygen saturation (SvO2) and SvO2 vs ScvO2
2018년 11월 7일 수요일
2018년 11월 6일 화요일
[CK] [ ] Arrhythmia followng OHT( no BB, no adenosine. just CCB!)
https://www.uptodate.com/contents/arrhythmias-following-cardiac-transplantation?search=cardiac%20transplant%20adenosine&source=search_result&selectedTitle=1~150&usage_type=default&display_rank=1
2018년 11월 5일 월요일
[CK] [] Post. MI vs Inferior MI
[CK] LBBB definition
- The heart rhythm must be supraventricular in origin
- The QRS duration must be ≥ 120 ms[2]
- There should be a QS or rS complex in lead V1
- There should be a notched ('M'-shaped) R wave in lead V6.
[CK] Flutter EKG - Typical vs Atypical []
Atrial rate ca. 300 bpm (200-400 bpm) with a heart rate typically ca. 150 bpm.
- Typical (type I) atrial flutter: saw-tooth-like waves
- Counterclockwise: negative flutter waves in II, III, aVF and positive in V1
- Clockwise: positive flutter waves in II, III, aVF and negative in V1
- Atypical (type II) atrial flutter: does not !
II III avF <-> V1 with SAW-TOOTH LIKE WAVES
2018년 11월 4일 일요일
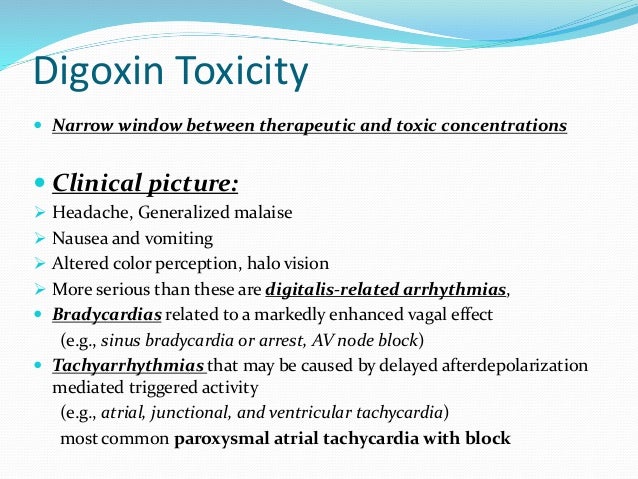
[ ] Please read!!!! [CK] Digoxin loading./ Digoxin toxicity(SX+ EKG - ANY TYPE but Smile or VT bigemmini)
[AFIB]
NO amio d/t liver failure.
THEN digoxin would be the only choice!!!!

(serum level of drug in approximately 7 to 10 days)
2. Rapid intravenous and oral digitalization can be used to control the ventricular response in AF and atrial flutter: Initial IV 0.25 to 0.5 mg of digoxin are given over several minutes, followed by 0.25 mg every six hours for a total dose of 0.75 to 1.5 mg with appropriate dosing adjustments for renal failure and the concomitant use of certain medications.
(IV infusion of 500-mcg -> Q6HR 250 -> upto 3 doses for total 1000mcg!!! )
(or 250 -> 125 -> 125 something like that as well.... - I would say medium rate?!)
(Renal, Digoxin level monitorring = as an OP?
REF> UPTODATE
Atrial fibrillation or atrial flutter, rate control (alternative agent) (off-label): Note: Some experts reserve digoxin for patients whose rate has not adequately been controlled with other agents or interventions (Ganz 2018; Giardina 2018). Additionally, digoxin is not effective for rate control during high-adrenergic states (eg, exercise); a beta-blocker is preferred (AHA/ACC/HRS [January 2014]).
Total digitalizing dose (TDD): Initial: IV: 8 to 12 mcg/kg (ideal/lean body weight); administer 50% of TDD over 5 minutes; administer the remaining 50% as 2 doses of 25% of TDD at 4- to 8-hour intervals after the initial dose (ACLS [Neumar 2011]) or may administer 0.25 to 0.5 mg over several minutes, with repeat doses of 0.25 mg every 6 hours to a maximum of 1.5 mg over 24 hours; follow either of these TDD regimens with an oral maintenance regimen (AHA/ACC/HRS [January 2014]; Giardina 2018).
Maintenance dose: Oral: 0.125 to 0.25 mg once daily (AHA/ACC/HRS [January 2014])
=====> 250 - 500 mcg -> 250 repeatedly!! (1000mcg and then 250 or 125 maintenance)
-
-
●Quinidine, verapamil, and amiodarone can increase serum digoxin levels, thereby requiring a reduction in the daily digoxin dose. Cholestyramine and antacids, on the other hand, can decrease the intestinal absorption of digoxin, necessitating spacing of the doses or an increase in the daily digoxin dose. In some patients, use of antibiotics such as tetracycline and erythromycin may impair gastrointestinal metabolism of digoxin, leading to higher serum digoxin concentrations. (See 'Dose adjustment with concomitant medications' above.)
Toxicity: HA, GI, BRADY(AV BLOCK) or TACHY(ATACH WITH BLOCK, JUNCTIONAL OR VT as well!)
EKG: Curved ST depression(SMILE SIGN of Digoxin's smile)
VT bigemmini
RISK: Hypokalemia => Even worse to change with this -> more activating Na-Ca exchanger! Going even further craziness !
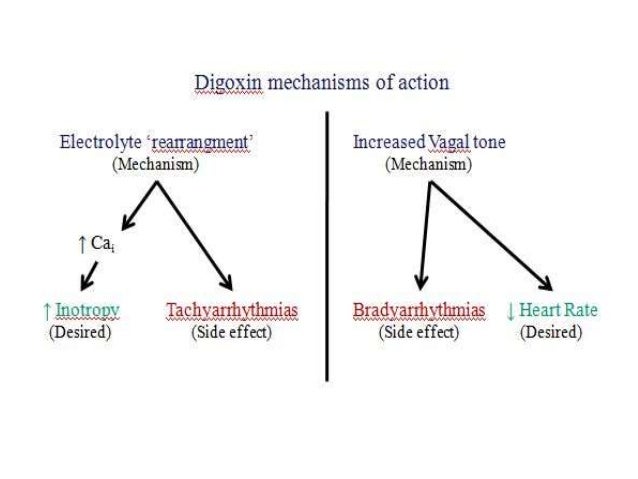
Pathophysiology
1. vasoconstriction in the arterial and venous system in vascular smooth muscle.
2. positive inotropic effect of digitalis has the following 2 components:
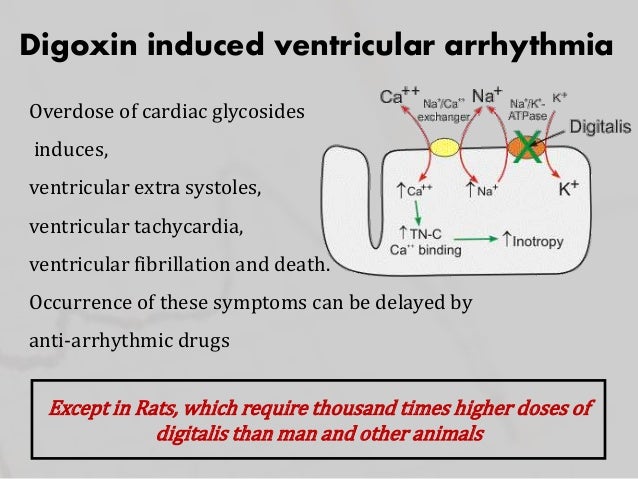
- Direct inhibition of membrane-bound sodium- and potassium-activated adenosine triphosphatase (Na+/K+ -ATPase), which leads to an increase in the intracellular concentration of calcium ([Ca2+]i); Na-K block -> Na-Ca activated !!!
- Associated increase in a slow inward calcium current (iCa) during the action potential (AP); this current is the result of movement of calcium into the cell, and it contributes to the plateau of the AP= Prolonged contraction.
Electrophysiologic effects???
The electrophysiological effects of cardiac glycosides include the following [8] :
- Decreased resting potential (RP) or maximal diastolic potential (MDP), which slows the rate of phase-0 depolarization and conduction velocity
- Decrease in action potential duration (APD), which results in increased responsiveness of fibers to electrical stimuli
- Enhancement of automaticity, which results from an increase in the rate of phase 4 depolarization and from delayed after-depolarization
- In general, cardiac glycosides slow conduction and increase the refractory period in specialized cardiac conducting tissue by stimulating vagal tone. Digitalis has parasympathetic properties, which include hypersensitization of carotid sinus baroreceptors and stimulation of central vagal nuclei.Digoxin also appears to have variable effects on sympathetic tone, depending on the specific cardiac tissue involved.
Dosage and toxicity; The kidney excretes 60-80% of the digoxin dose unchanged. Kidney injury + Hypokalemia = WORST COMBINATION !!
The onset of action after oral (PO) administration occurs in 30-120 minutes; the onset of action with intravenous (IV) administration occurs in 5-30 minutes. At therapeutic levels, the elimination half-life is 36 hours. IDysrhythmias
Alterations in cardiac rate and rhythm from digitalis toxicity may simulate almost every known type of dysrhythmia. Although no dysrhythmia is pathognomonic for digoxin toxicity, toxicity should be suspected when evidence of increased automaticity and depressed conduction is noted. +cumulative results of the direct, vagotonic, and antiadrenergic actions of digitalis.==============================================================================================================The effects of digoxin vary with the dose and differ depending on the type of cardiac tissue involved. The atria and ventricles exhibit increased automaticity and excitability, resulting in extrasystoles and tachydysrhythmias. Conduction velocity is reduced in myocardial and nodal tissue, resulting in increased PR interval and AV block accompanied by a decrease in the QT interval.In addition to these effects, the direct effect of digitalis on repolarization often is reflected in the electrocardiogram (ECG) by ST segment and T-wave forces opposite in direction to the major QRS forces. The initial electrophysiologic manifestation of digitalis effects and toxicity usually is mediated by increased vagal tone.Early in acute intoxication, depression of sinoatrial (SA) or AV nodal function may be reversed by atropine. Subsequent manifestations are the result of direct and vagomimetic actions of the drug on the heart and are not reversed by atropine.Ectopic rhythms are due to enhanced automaticity, reentry, or both, and may include the following:- Nonparoxysmal junctional tachycardia
- Extrasystole
- Premature ventricular contractions
- Ventricular flutter and fibrillation
- Atrial flutter and fibrillation
- Bidirectional ventricular tachycardia
Bidirectional ventricular tachycardia is particularly characteristic of severe digitalis toxicity and results from alterations in intraventricular conduction, junctional tachycardia with aberrant intraventricular conduction, or, on rare occasions, alternating ventricular pacemakers.The following features may also be seen:- Depression of the atrial pacemakers, resulting in SA arrest
- SA block
- AV block
- Sinus exit block resulting from depression of normal conduction
- Nonparoxysmal atrial tachycardia with block
When conduction and the normal pacemaker are both depressed, ectopic pacemakers may take over, producing atrial tachycardia with AV block and nonparoxysmal automatic AV junctional tachycardia. Indeed, AV junctional blocks of varying degrees, alone or with increased ventricular automaticity, are the most common manifestations of digoxin toxicity, occurring in 30-40% of cases. AV dissociation may result from suppression of the dominant pacemaker with escape of a subsidiary pacemaker or inappropriate acceleration of a ventricular pacemaker.Arrhythmias can cause inadequate tissue perfusion, with resultant central nervous system (CNS) and renal complications, such as the following:- Hypoxic seizures
- Encephalopathies
- Loss of vasoregulation
- Acute tubular necrosis
Hyperkalemia is the major electrolytic complication in acute, massive digoxin poisoning. In pediatric patients, hyperkalemia can be a complication of acute toxicity.
ADDITIONAL LECTURE in YOUTUBE >>>
Digoxin therapeutic EKG: ST depression(salvadore dali), T flat, QT shortening(hypercalcemia)
Toxic EKG: TWI, Sinus brady, AV block
PAT, VT, PVC, Bigemminy
Interaction: amiodarone, verapamil
and PPI(will increase effect) <-> H2 blocker(will decrease effect)
Goal: 0.5 - 0.9
Stablization: 7d - 10d
effect: inotropic,
higher vagal tone to SA, AV node. (slow down)
avoid: hypokalemia(higher change to have arrhythmia)
https://www.youtube.com/watch?v=EpeLXRlFI1I
피드 구독하기:
덧글 (Atom)