[AFIB]
NO amio d/t liver failure.
THEN digoxin would be the only choice!!!!

(serum level of drug in approximately 7 to 10 days)
2. Rapid intravenous and oral digitalization can be used to control the ventricular response in AF and atrial flutter: Initial IV 0.25 to 0.5 mg of digoxin are given over several minutes, followed by 0.25 mg every six hours for a total dose of 0.75 to 1.5 mg with appropriate dosing adjustments for renal failure and the concomitant use of certain medications.
(IV infusion of 500-mcg -> Q6HR 250 -> upto 3 doses for total 1000mcg!!! )
(or 250 -> 125 -> 125 something like that as well.... - I would say medium rate?!)
(Renal, Digoxin level monitorring = as an OP?
REF> UPTODATE
Atrial fibrillation or atrial flutter, rate control (alternative agent) (off-label): Note: Some experts reserve digoxin for patients whose rate has not adequately been controlled with other agents or interventions (Ganz 2018; Giardina 2018). Additionally, digoxin is not effective for rate control during high-adrenergic states (eg, exercise); a beta-blocker is preferred (AHA/ACC/HRS [January 2014]).
Total digitalizing dose (TDD): Initial: IV: 8 to 12 mcg/kg (ideal/lean body weight); administer 50% of TDD over 5 minutes; administer the remaining 50% as 2 doses of 25% of TDD at 4- to 8-hour intervals after the initial dose (ACLS [Neumar 2011]) or may administer 0.25 to 0.5 mg over several minutes, with repeat doses of 0.25 mg every 6 hours to a maximum of 1.5 mg over 24 hours; follow either of these TDD regimens with an oral maintenance regimen (AHA/ACC/HRS [January 2014]; Giardina 2018).
Maintenance dose: Oral: 0.125 to 0.25 mg once daily (AHA/ACC/HRS [January 2014])
=====> 250 - 500 mcg -> 250 repeatedly!! (1000mcg and then 250 or 125 maintenance)
-
-
●Quinidine, verapamil, and amiodarone can increase serum digoxin levels, thereby requiring a reduction in the daily digoxin dose. Cholestyramine and antacids, on the other hand, can decrease the intestinal absorption of digoxin, necessitating spacing of the doses or an increase in the daily digoxin dose. In some patients, use of antibiotics such as tetracycline and erythromycin may impair gastrointestinal metabolism of digoxin, leading to higher serum digoxin concentrations. (See 'Dose adjustment with concomitant medications' above.)
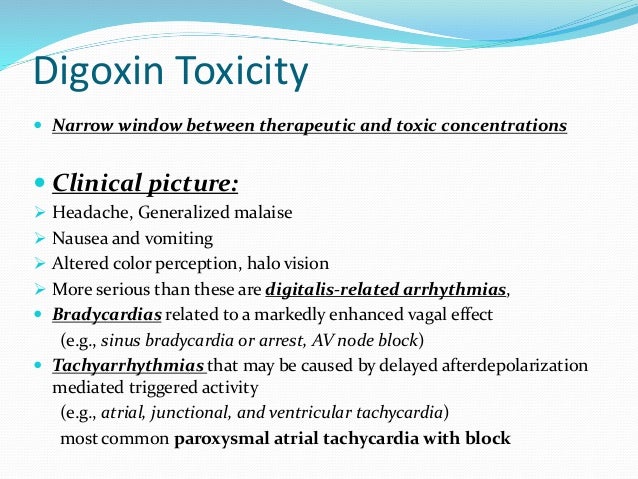
Toxicity: HA, GI, BRADY(AV BLOCK) or TACHY(ATACH WITH BLOCK, JUNCTIONAL OR VT as well!)
EKG: Curved ST depression(SMILE SIGN of Digoxin's smile)
VT bigemmini
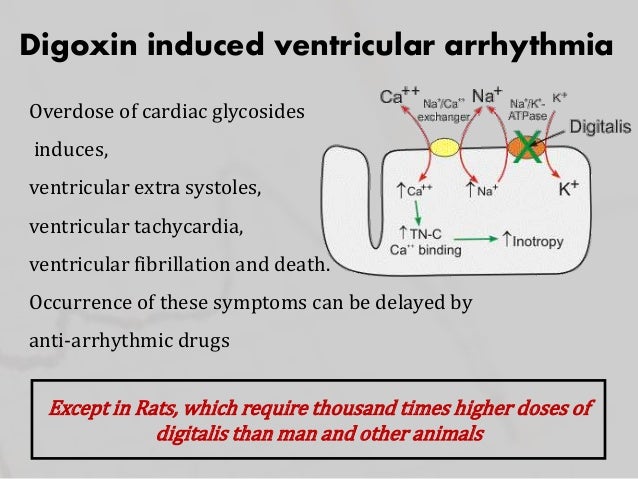
RISK: Hypokalemia => Even worse to change with this -> more activating Na-Ca exchanger! Going even further craziness !
Pathophysiology
1. vasoconstriction in the arterial and venous system in vascular smooth muscle.
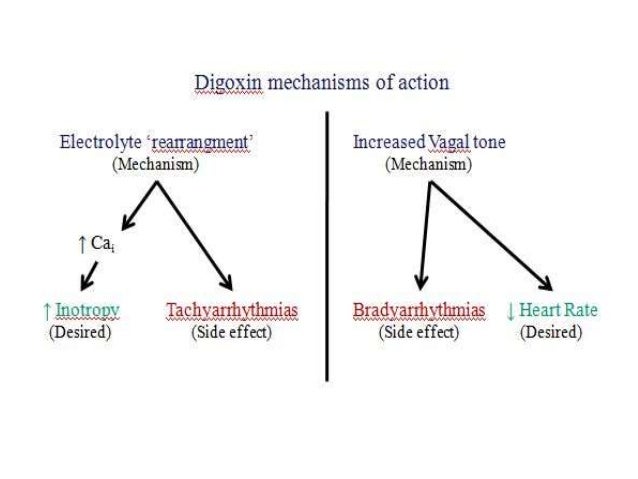
2. positive inotropic effect of digitalis has the following 2 components:
- Direct inhibition of membrane-bound sodium- and potassium-activated adenosine triphosphatase (Na+/K+ -ATPase), which leads to an increase in the intracellular concentration of calcium ([Ca2+]i); Na-K block -> Na-Ca activated !!!
- Associated increase in a slow inward calcium current (iCa) during the action potential (AP); this current is the result of movement of calcium into the cell, and it contributes to the plateau of the AP= Prolonged contraction.
Electrophysiologic effects???
The electrophysiological effects of cardiac glycosides include the following [8] :
- Decreased resting potential (RP) or maximal diastolic potential (MDP), which slows the rate of phase-0 depolarization and conduction velocity
- Decrease in action potential duration (APD), which results in increased responsiveness of fibers to electrical stimuli
- Enhancement of automaticity, which results from an increase in the rate of phase 4 depolarization and from delayed after-depolarization
- In general, cardiac glycosides slow conduction and increase the refractory period in specialized cardiac conducting tissue by stimulating vagal tone. Digitalis has parasympathetic properties, which include hypersensitization of carotid sinus baroreceptors and stimulation of central vagal nuclei.Digoxin also appears to have variable effects on sympathetic tone, depending on the specific cardiac tissue involved.
Dosage and toxicity; The kidney excretes 60-80% of the digoxin dose unchanged. Kidney injury + Hypokalemia = WORST COMBINATION !!
The onset of action after oral (PO) administration occurs in 30-120 minutes; the onset of action with intravenous (IV) administration occurs in 5-30 minutes. At therapeutic levels, the elimination half-life is 36 hours. IDysrhythmias
Alterations in cardiac rate and rhythm from digitalis toxicity may simulate almost every known type of dysrhythmia. Although no dysrhythmia is pathognomonic for digoxin toxicity, toxicity should be suspected when evidence of increased automaticity and depressed conduction is noted. +cumulative results of the direct, vagotonic, and antiadrenergic actions of digitalis.==============================================================================================================The effects of digoxin vary with the dose and differ depending on the type of cardiac tissue involved. The atria and ventricles exhibit increased automaticity and excitability, resulting in extrasystoles and tachydysrhythmias. Conduction velocity is reduced in myocardial and nodal tissue, resulting in increased PR interval and AV block accompanied by a decrease in the QT interval.In addition to these effects, the direct effect of digitalis on repolarization often is reflected in the electrocardiogram (ECG) by ST segment and T-wave forces opposite in direction to the major QRS forces. The initial electrophysiologic manifestation of digitalis effects and toxicity usually is mediated by increased vagal tone.Early in acute intoxication, depression of sinoatrial (SA) or AV nodal function may be reversed by atropine. Subsequent manifestations are the result of direct and vagomimetic actions of the drug on the heart and are not reversed by atropine.Ectopic rhythms are due to enhanced automaticity, reentry, or both, and may include the following:- Nonparoxysmal junctional tachycardia
- Extrasystole
- Premature ventricular contractions
- Ventricular flutter and fibrillation
- Atrial flutter and fibrillation
- Bidirectional ventricular tachycardia
Bidirectional ventricular tachycardia is particularly characteristic of severe digitalis toxicity and results from alterations in intraventricular conduction, junctional tachycardia with aberrant intraventricular conduction, or, on rare occasions, alternating ventricular pacemakers.The following features may also be seen:- Depression of the atrial pacemakers, resulting in SA arrest
- SA block
- AV block
- Sinus exit block resulting from depression of normal conduction
- Nonparoxysmal atrial tachycardia with block
When conduction and the normal pacemaker are both depressed, ectopic pacemakers may take over, producing atrial tachycardia with AV block and nonparoxysmal automatic AV junctional tachycardia. Indeed, AV junctional blocks of varying degrees, alone or with increased ventricular automaticity, are the most common manifestations of digoxin toxicity, occurring in 30-40% of cases. AV dissociation may result from suppression of the dominant pacemaker with escape of a subsidiary pacemaker or inappropriate acceleration of a ventricular pacemaker.Arrhythmias can cause inadequate tissue perfusion, with resultant central nervous system (CNS) and renal complications, such as the following:- Hypoxic seizures
- Encephalopathies
- Loss of vasoregulation
- Acute tubular necrosis
Hyperkalemia is the major electrolytic complication in acute, massive digoxin poisoning. In pediatric patients, hyperkalemia can be a complication of acute toxicity.
ADDITIONAL LECTURE in YOUTUBE >>>
Digoxin therapeutic EKG: ST depression(salvadore dali), T flat, QT shortening(hypercalcemia)
Toxic EKG: TWI, Sinus brady, AV block
PAT, VT, PVC, Bigemminy
Interaction: amiodarone, verapamil
and PPI(will increase effect) <-> H2 blocker(will decrease effect)
Goal: 0.5 - 0.9
Stablization: 7d - 10d
effect: inotropic,
higher vagal tone to SA, AV node. (slow down)
avoid: hypokalemia(higher change to have arrhythmia)
https://www.youtube.com/watch?v=EpeLXRlFI1I
댓글 없음:
댓글 쓰기